Sept 2025- KDIGO released yet another IgAN Guidelines. The last one was in 2021. Since 2021, several new trials were published with novel agents to be used in IgAN-- from Nefecon, Sparsenten, Atrasenten and Iptacopan. Which ones made this new guideline?
This is the main figure from the guidelines.
The key takeaways
1. In all patients, treatment of the immunological side of IgAN and the CKD side, at the same time
2. Addition of Nefecon as an alternative to Steroids
3. Addition of DEARA and SGLT2i to the main CKD treatment option.
4. Lower proteinuria goal of 0.5g/day or lower and ideally 0.3g/day. and a stable eGFR
5. Early renal biopsy encouragement
6. Still consider clinical trials in the right cases.
Few misses
1. Pure endothlin antagonists -- will they have a role?
2. Why did complement inhibition not make this cut... perhaps waiting for long-term data
3. APRIL inb soone to be approved and may even add a dent to this strategy above.




















 Pauci immune focal and segmental necrotizing GN guidelines by KDIGO
Pauci immune focal and segmental necrotizing GN guidelines by KDIGO
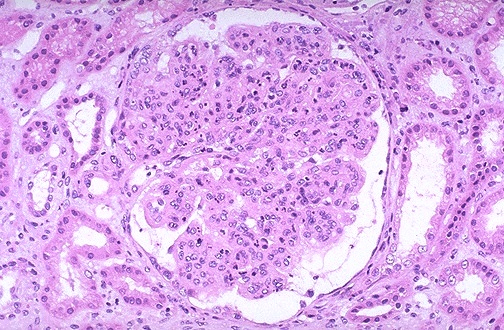
 KDIGO guidelines are proposed this year in recent Kidney International on glomerular disease.
KDIGO guidelines are proposed this year in recent Kidney International on glomerular disease. KDIGO released guidelines in glomerular diseases in a Kidney International supplement this year.( image source: RFN)
KDIGO released guidelines in glomerular diseases in a Kidney International supplement this year.( image source: RFN)