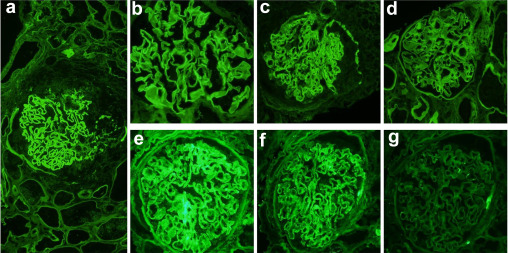
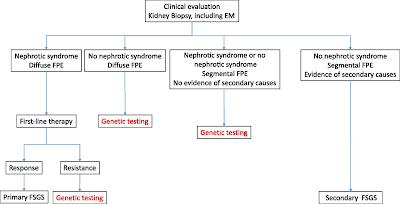
Recent advances have reshaped how we view nephrotic syndrome moving from descriptive pathology to a mechanism-based model. A growing body of evidence shows that circulating autoantibodies against key slit diaphragm proteins—nephrin, podocin, and Kirrel1—play a central role in many cases of autoimmune podocytopathy. This was also confirmed in pediatric literature.
These discoveries promise earlier, less invasive diagnosis and more precise, personalized treatment.
Yet, translating these insights into clinical practice is far from straightforward. The antibodies are often present at very low or transient levels, disappearing into the urine during active disease. Their titers fluctuate with relapses and remissions, complicating the timing of tests. Moreover, NS is heterogeneous: while many patients have anti-nephrin antibodies, others harbor antibodies to podocin or Kirrel1, and some exhibit overlapping profiles through “epitope spreading.”
Technical challenges also hamper detection. Assay performance depends on antigen fragment choice, expression system, and protein modifications—especially for the heavily glycosylated nephrin. To improve reliability, researchers emphasize combined strategies, pairing ELISA with high-resolution biopsy techniques like super-resolution microscopy.
The article proposes a roadmap: develop multiplex assays, standardize antigen design, integrate biopsy validation, and pursue longitudinal studies. Success could enable precision diagnostics and tailored therapy, transforming care for children and adults with nephrotic syndrome.
Is it time for targeted therapies for Glomerular Diseases?

.png)