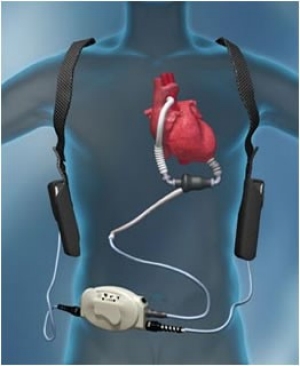
Should patients on dialysis or kidney
transplant be offered LVADS for severe CHF?
A new study just published in JAMA internal Medicine showed that patients with ESRD at the time of LVAD placement had an extremely poor prognosis, with most surviving for less than 3 weeks.
A new study just published in JAMA internal Medicine showed that patients with ESRD at the time of LVAD placement had an extremely poor prognosis, with most surviving for less than 3 weeks.
This was a observational analysis of the
USRDS data of all patients on ESRD that received an LVAD. 155 Medicare beneficiaries with ESRD (median
and interquartile range [IQR] days from ESRD onset to LVAD placement were 1655
days [453-3050 days]) and 261 beneficiaries without ESRD in the Medicare 5%
sample received an LVAD. During a median follow-up of 762 days, 127 patients
(81.9%) with and 95 (36.4%) without ESRD died. More than half of patients with
ESRD (80 [51.6%]) compared with 11 (4%) of those without ESRD died during the
index hospitalization. The median time to death was 16 days for patients with
ESRD compared with 2125 days for those without ESRD. Most of these patients
were hemodialysis with a small minority being PD and transplantation. So,
unclear what the data is for PD vs transplantation.
In addition, what would have happened if the
patients continued conservative management and not offered LVAD- would their
outcomes have been similar or better? This really brings the question on
whether LVADS should be offered to ESRD patients on dialysis.