The recent KDIGO guidelines are here
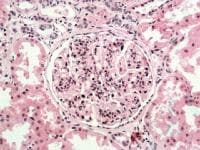
One of the most important changes is getting rid of the MPGN1, 2 and 3 classification and using the novel pathophysiology based classification and recognizing that MPGN is a pattern of injury
The diagnosis of the C3GN and DDD is tough and requires the extensive assays and testing on complement cascade.
For idiopathic causes of MPGN pattern of injury, consider a limited course of steroids
For RPGN of idiopathic cause, steroids + cyclophosphamide
For MPGN with low GFR< 30, supportive treatment only
For C3GN, and no signs of MGRS, and failed MMF and steroids, eculizumab should be considered




 KDIGO guidelines are proposed this year in recent Kidney International on glomerular disease.
KDIGO guidelines are proposed this year in recent Kidney International on glomerular disease.