Saturday, August 30, 2025
Thursday, March 14, 2024
In the News: Dense Deposit Disease and ApoE- the new connection
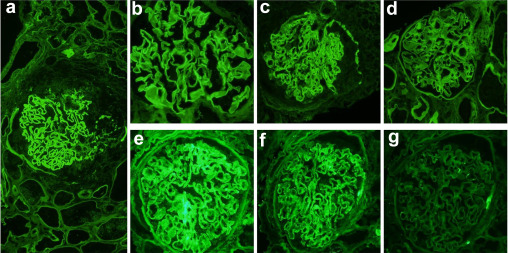
C3 glomerulopathy arises from irregularities in the alternative pathway of complement. It manifests as two types: C3 glomerulonephritis (C3GN) and dense deposit disease (DDD), identifiable by bright C3 staining in the glomeruli under immunofluorescence. EM distinguishes DDD by dense deposits along the glomerular basement membranes, contrasting with non-dense deposits in C3GN. A fascinating new study investigating 12 cases each of DDD, C3GN, and pretransplant kidney controls, laser microdissection (LCM) followed by mass spectrometry (MS) revealed a significant accumulation of complement proteins and regulatory factors in both C3GN and DDD compared to controls. Notably, DDD exhibited a much higher concentration of C5-9 and apolipoprotein E (ApoE) compared to C3GN.
Image courtesy: pathologyoutlines.com
ApoE staining aligned with dense deposit patterns in DDD but not in C3GN or controls, validated in 31 C3G cases. This is fascinating as perhaps ApoE staining may serve as a diagnostic tool for DDD, particularly when EM is unavailable, as it reflects the enriched presence of ApoE in dense deposits, distinguishing DDD from C3GN.
Saturday, February 24, 2024
CONSULT ROUNDS: NELL-1 MEMBRANOUS NEPHROPATHY
After PLA2R, NELL-1 related membranous nephropathy(MN) seems to be the second most common MN. Initially, the studies had pointed towards a cancer-related cause for NELL-1 MN. In recent years and most recently, 2 papers published in 2024 highlight the role of complementary medications.
A study from India investigates the clinical outcomes of NELL1-associated MN compared to unidentified antigen-associated MN. Among 46 NELL1 and 36 unidentified antigen-associated MN patients, a significant history of complementary and alternative medicine (CAM) use was noted particularly in the NELL1 group. NELL1-associated MN patients showed a lesser need for immunosuppression, attributed partly to CAM intake, with similar remission rates observed in both groups. The study highlights the distinct clinical features of NELL1-associated MN, including its association with CAM, and suggests a potential for spontaneous remission in these patients. Despite limitations like small sample size and short follow-up, findings indicate CAM's role in NELL1-associated MN and underscore the need for further research in this entity.
A study spanning three institutions in the USA reviewed NELL1 associated MN cases, revealing that 53% of the 70 patients were male, with a median age of 66 and proteinuria of 5.9 grams/day. Associations included lipoic acid (36%), heavy NSAID use (27%), autoimmune diseases (23%), and malignancy (33%). At a median 11-month follow-up, 72% achieved remission, notably 91% in lipoic acid-associated cases with ≥6 months follow-up. Primary NELL1 MN and greater tubular atrophy and interstitial fibrosis predicted lower remission rates, while lipoic acid use correlated with higher complete remission rates, suggesting its discontinuation as a primary treatment strategy.
I have revised my concept map for NELL-1 MN based on this study to really highlight the CAM and Lipoic acid components. ( created using bio-render).
Saturday, April 29, 2023
Topic Discussion: Atypical anti GBM disease
We are aware that circulating anti-GBM antibodies are directly pathogenic in anti-GBM disease. However, about 10% of patients with anti-GBM disease do not have circulating anti- GBM antibodies.
Atypical anti-GBM disease is considered when patients have linear IgG deposition along the glomerular basement membrane without anti-GBM antibodies in the circulation.
Atypical anti-GBM disease comprises 8% to 12% of all anti-GBM disease cases. About 2% to 8% of patients with anti-GBM disease have negative serology despite rigorous testing.
Pathogenesis:
(1)different composition of antigen/epitope: a)Antibodies against the NC1 domain of other alpha chains like alpha1, alpha4, or alpha5 chains of type IV collagen or to the NC1 domain of alpha345 hexamers, b)Linear epitopes of the collagenous domain, or C)entactin
(2)different affinity of antibodies: a) high-affinity autoantibodies trapped in the kidneys and present with low titer in circulation, or (b)Autoantibodies could also have a low affinity for the substrate in the assay
(3) different types of antibody: a). the dominance of different IgG subclass such as IgG4 or IgG1 and frequent presence of IgG2, b) presence of IgA or IgM dominance which is not exactly atypical anti-GBM diseases in terms of clinical/pathological presentation
Pathology: (i) Lack diffuse crescentic and necrotizing glomerulonephritis, (ii). Light microscopy heterogenous: mesangial and/or endocapillary proliferative GN, MPGN, FSGS, mesangial sclerosis; and glomerular endothelial changes resembling TMA are common
Monotypic atypical anti-GBM disease: Monotypic Ig deposits along the GBM are increasingly observed to cause a disease pattern similar to atypical anti-GBM. Needs further study to confirm if it is a form of MGRS?
Prognosis: Kidney dysfunction is usually milder and evolves slower than classic anti-GBM disease; however, presentation as RPGN has also been reported. Proteinuria and nephrotic syndrome are more frequent than classic anti-GBM disease.
Treatment: is individualized and typically consists of immunosuppressive agents used to treat classic anti-GBM disease or monotherapy with renin-angiotensin-aldosterone blockers
Saturday, February 25, 2023
Golden Era in therapeutics for IgA Nephropathy
Just in the last 1 year, we have two new drugs being approved for IgA Nephropathy. In addition, we have seen an emergence in using SGLT2i perhaps in IgAN and other GNs. The DAPA-CKD trial IgAN patients were evaluated and the use of dapagliflozin was superior than placebo. The EMPA-Kidney had close to 800 IgAN patients, we shall await those results soon.
MMF has just made a come back with a recent Chinese study showing some promise in a RCT.
Finally, a targeted release steroid called budesonide has been FDA approved. This was developed to deliver the active drug in the distal ileum, where the Peyer's patches are -- the likely culprit where a large amount of galactose deficient IgA is made. The data was just published in KI.
And finally, the first single molecule Dual Endothelin Angiotensin Receptor Antagonist (DEARA) approved for use in patients with IgAN. The data is not published yet in a journal.
There are still ongoing trials of other DEARAs, and complement inhibitors, APRIL inhibitors for IgAN. In my opinion, the future of treatment of IgAN can be perhaps summarized in the below figure: ( created using biorender.com)
Friday, January 6, 2023
NELL-1 Membranous Nephropathy- Concept Map
This is an inspired figure from Sethi's amazing review in CKJ.
This figure is a summary of the various secondary causes of NELL-1 MN that have been described.
( keeping in mind that primary NELL-1 MN without a secondary cause still is the most common)
Saturday, August 20, 2022
GN Chat- a new initiative
The Glomerular Center of Northwell now runs a special monthly GN chat to discuss fun and interesting case based discussions of glomerular disease topics. This is on 3rd Tuesday of each month at 8AM EST
Register in advance for this meeting:
https://northwell.zoom.us/meeting/register/tJElf-iqqzgoE9edbml-AI1dNR07Q1LQOL-m
After registering, you will receive a confirmation email containing information about joining the meeting.
Come learn GN in a coffee style manner with experts in the field- Purva Sharma, Jordan Rosenstock and Kenar Jhaveri
Friday, July 22, 2022
New Combined Glomerular Diseases and Onco-Nephrology Fellowship at Northwell
Northwell Nephrology is offering both a traditional two year general nephrology fellowship as well as a new fellowship that includes a third year fellowship specializing in glomerular diseases and onconephrology. The traditional two year fellowship can be applied for through this link
A candidate for the Galdi Fellowship will have completed internal medicine residency training, a general nephrology fellowship and demonstrate the highest level of performance and scientific and clinical potential. Candidates for the Galdi Fellowship would be carefully vetted based upon academic and other indications suggesting that advanced training as a Galdi Fellow would enable their ability to become one of a select few international leaders in glomerular diseases and onco-nephrology. The Galdi Fellowship will last for one academic calendar (July through June) year. A new fellow will be recruited each year.
Training in glomerular kidney diseases is through the Northwell Nephrology Center for Glomerular Diseases directed by Drs. Kenar Jhaveri and Purva Sharma. The fellow will work in the Glomerular Disease Center and be exposed to all aspects of glomerular disease management including a rotation with Division of Rheumatology for extra training in SLE and ANCA vasculitis. The fellow will also have the opportunity to participate in ongoing clinical trials in glomerulonephritis at the Glomerular Disease Center.
Onconephrology overlaps to an extent with glomerular diseases. Fellows gain experience both in the clinic and hospital with world renowned leaders Rimda Wanchoo and Kenar Jhaveri. Rotations will also include with hematology and oncology teams dealing with multiple myeloma, renal cell cancer and bone marrow transplant services. In addition, the fellow will have rotations with our nephropathologists as well.
Currently we are accepting applications from current nephrology fellows or recent graduates for the Galdi Fellowship for start date of July 2023. In addition we are accepting applications from internal medicine residents for the general nephrology fellowship starting July, 2023 with a third year Galdi fellowship starting in July, 2025.
For inquiries regarding the advanced fellowship program, please email Dr. Kenar Jhaveri at kjhaveri@northwell.edu
The application should include
1. CV of the applicant
2. Two recommendation letters (one must be from the Nephrology Program Director of Chief)
3. A Personal Statement on the reasons for joining this fellowship.
Friday, July 8, 2022
Opinion- Renal Thrombotic Microangiopathy?- Should we be calling it Renal Limited Endothelial injury or Endothelial Injury of Renal Significance
Thrombotic Microangiopathy- what’s in a name?
This is a common conversation:
“ The kidney biopsy confirms TMA”. Great- we should ask hematology to help
treat..
Hematology—“ but there are no signs of microangiopathic hemolytic anemia.. no schistocytes
on smear—no need to treat”
Another conversation
“ The kidney biopsy confirms TMA”. But there are no micro thrombi on the kidney biopsy.
This is likely from HTN—treat the HTN. “
but the patient has a complement factor H mutation..”.. hmm..
The presentation of TMA can be as mild as HTN only, or AKI
on CKD or HTN with CKD or nephritic syndrome or nephrotic syndrome or just
nephrotic range proteinuria with AKI. The clinical presentation is very varied.
I have seen it all.
The problem with TMA starts with the nomenclature. Personally, I have a problem with a series of
diseases in the kidney called TMA—some have angiopathy only, some have
endotheliosis, some have both and some have additional microthrombi but at the
end we call all of them TMA.
Most of TMA cases are without thrombosis, only rarely would
you see true thrombi. Frank thrombosis
is more common in (catastrophic) APLAS associated TMA in the kidney.
Some TMA tends to be more glomerular classically in pregnancy related, for example,
with endothelial cell swelling = endotheliosis). And some TMA tends to be more arterial
(thrombotic angiopathy rather than microangiopathy). Or we might be
catching them at various points in time. A continuous process..
The pathology is also variable and hence should be considered to be defined perhaps with what is noted on it.
Endothelial injury with angiopathy
Endothelial injury with micro thrombi
Endothelial injury with endotheliosis predominant
The cause of the injury than can be defined better based on
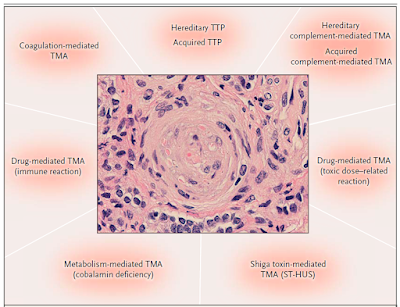
history of the patient and then divided into categories as per the syndromes of
TMA or better called “endothelial injury”- such as ADAMTS13 mediated, complement
mediated, Drug induced ( immune vs toxic), Shiga toxin mediated, metabolism
mediated, coagulation mediated and so forth. This figure is from the classic NEJM article by George et al in 2014.
As we learn more about renal endothelial injury, perhaps a better practical terminology may be useful in defining the disease to help clinicians guide the treatment plan.
Monday, June 6, 2022
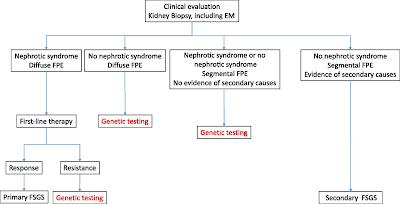
Topic Discussion: Ever changing FSGS classifications
FSGS is a tough diagnosis and often confusing to the Nephrologist. Classifications in FSGS also have been very confusing and challenging. Several years ago, the pathology based classification had entered all textbooks.
Is this classification clinically useful? Not sure it is to most nephrologists? If I have a tip variant FSGS, or Perihilar, does it tell me anything re the cause and outcome? Maybe- but mostly not.
In 2007, there was a movement towards changing the concept to more podocytopathy based. ( see below- recreated using biorender).
Not sure if this is useful either but it really asked a fundamental question re how we are seeing these spectrum of diseases we term FSGS.
The most useful to me personally is classifying the FSGS presentation into
1) primary vs secondary cause
2) nephrotic syndrome vs nephrotic range proteinuria
While not 100% in most cases, nephrotic syndrome and FSGS usually is going to have a primary cause( sparing some genetic causes and viruses). In addition, what is also helpful from a pathology standpoint is not the LM, but the EM--
3) Is there diffuse or partial foot process effacement?- Usually the former responds to treatment better with steroids or other immunosuppression and later is more likely a secondary cause. It may also aid in looking for a secondary cause.
This figure from a JASN paper by De Vriese et al is very helpful indeed.
So FSGS really should be described more in terms of primary vs secondary causes and EM findings to help in treatment decisions. Classically, your "permeability or immune mediated" FSGS should respond to treatment and would fit under nephrotic syndrome, diffuse foot process effacement and classically your primary FSGS. Secondary FSGS from various causes like low nephron mass, obesity, viral , meds- all classically would have nephrotic range proteinuria and sporadic foot process effacement on EM. That being said, some genetic causes of FSGS would be seen to have diffuse foot process effacement as well. Genetic FSGS is an important one to keep in mind and screening for genetic causes should be done: young patient, family hx, resistant to treatment, aiding in post transplant risk. etc.
KDIGO GN 2021 guidelines summarize this nicely
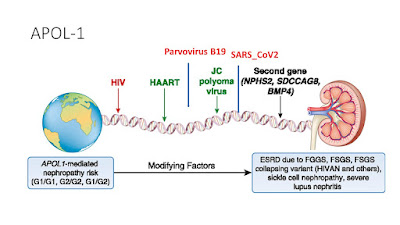
APOL-1 plays an important cause and role here and this slide can summarize the primary and the second hit concept with APOL-1 related FSGS
We should not forget --nonspecific scarring on renal biopsies. FSGS should also be differentiated from focal segmental scarring that develops in immune-mediated GN (e.g., Membranous Nephropathy, IgA Neph, ANCA-associated GN, and lupus nephritis) as a result of post-inflammatory scarring of necrotizing or proliferative lesions. This happens a lot and this should not be treated as FSGS.
In summary, FSGS has come a long way and finally we are seeing some changes in the way we are describing it.. Best 3 ways to categorize FSGS is clinically and EM based.
1. Primary vs Secondary
2. Nephrotic syndrome vs nephrotic range proteinuria
3. Diffuse foot process effacement vs partial foot process effacement
Tuesday, November 23, 2021
KDIGO 2021- GN Management Guidelines: MPGN
The recent KDIGO guidelines are here
One of the most important changes is getting rid of the MPGN1, 2 and 3 classification and using the novel pathophysiology based classification and recognizing that MPGN is a pattern of injury
For idiopathic causes of MPGN pattern of injury, consider a limited course of steroids
For RPGN of idiopathic cause, steroids + cyclophosphamide
For MPGN with low GFR< 30, supportive treatment only
For C3GN, and no signs of MGRS, and failed MMF and steroids, eculizumab should be considered
Thursday, October 28, 2021
KDIGO 2021- GN Management Guidelines: Infection associated GN
Bacterial infection associated GN- 4 main types
Post infectious GN
Shunt nephritis
Endocarditis associated GN
IgA dominant infection related GN
All 4 of them usually have low complement levels. No RCT for treatment
Antibiotics or surgical treatment for respective infections
Viral infection associated GN-
Hep B- Hep B DNA >2000 IU/ml, need treatment with anti Hep B agent and no avoid immunosuppressive agents as can accelerate the viral infection.
HIV disease: HAART therapy is recommended for all HIVAN and HIVICK diseases.
Hep C associated GN: A kidney biopsy should be performed in HCV-positive patients with clinical evidence of glomerular disease. Patients with mild or moderate forms of HCV-associated GN with stable kidney function and/or non-nephrotic proteinuria should be managed first with a DAA regimen. Patients with severe cryoglobulinemia or severe glomerular disease induced by HCV (i.e., nephrotic proteinuria or rapidly progressive kidney failure) should be treated with immunosuppressive agents (generally with rituximab as the first-line agent) and/or plasma exchange in addition to DAA therapies. Patients with HCV-related glomerular disease who do not respond to or are intolerant of antiviral treatment should also be treated with immunosuppressive agents.
Monday, October 25, 2021
KDIGO 2021- GN Management Guidelines: FSGS
FSGS has been the waste basket diagnosis for years. KDIGO finally has adopted the primary vs secondary FSGS way of thinking to make it easier to treat FSGS and diagnose the 99% of the secondary causes. Check out these amazing figures from the supplement
After 6 months, no response- considering MMF, anti cd20 agents but data on both is small.
Thursday, October 21, 2021
KDIGO 2021: GN Management Guidelines: Membranous Nephropathy
MN management has changed in 2020 onwards thanks to two trials published in 2020-2021 that showed that cyclophosphamide/steroids is superior and rituximab is not the main player yet.
The figures below summarize the main points of the GN 2021 KDIGO update
Monday, October 18, 2021
KDIGO 2021: GN Management Guidelines: IgA nephropathy
Does immunosuppressive meds help IgA nephropathy? Do we await the budesonide directed therapy approval, do we await more supportive agents such as ET1 antagonists or Aldo antagonists? Time will tell. Till then, IgA nephropathy is still the hardest GN to treat as we don't have clear options for treating the pathophysiology of the disease.
Saturday, September 11, 2021
Hypocomplementemia and the Kidney
When we are faced with AKI and classically low c3 and c4, certain diseases come to mind.
Monday, May 17, 2021
COVID19 vaccine induced glomerular diseases?- a literature update May 2021
The vaccine for COVID19 has been a lifesaver for many around the world. As expected, as you upregulate your immune system- you are going to get some flare ups of your immune system. Thus far, what are we noticing Minimal change disease, MN and IgA nephropathy.
Several published cases of podocytopathies- mainly minimal change disease- either de-novo or relapse have been reported ( 4 cases thus far)
https://www.kidney-international.org/article/S0085-2538(21)00493-2/fulltext (Pfizer-BioNTech )
https://www.sciencedirect.com/science/article/pii/S0272638621005096 (Pfizer-BioNTech)
https://www.ajkd.org/article/S0272-6386(21)00602-8/fulltext ( Pfizer-BioNTech )
https://www.kidney-international.org/article/S0085-2538(21)00478-6/fulltext (Pfizer-BioNTech)
IgA nephropathy flaring up has been reported ( 3 cases thus far)
https://www.kidney-international.org/article/S0085-2538(21)00465-8/fulltext ( Moderna)
https://www.kidney-international.org/article/S0085-2538(21)00286-6/fulltext (Moderna)
Relapse of Membranous Nephropathy ( one case)
https://www.kidney-international.org/article/S0085-2538(21)00494-4/fulltext (Sinovac’s COVID-19 vaccine.)
Acute transplant rejection has been reported
https://www.kidney-international.org/article/S0085-2538(21)00466-X/fulltext ( Pfizer-BioNTech)
While we cannot be totally sure if this is vaccine related- timing maybe a factor. I am sure there will be many more to be added to this list.
Despite this, the vaccine saves lives! Remember severe COVID19 disease led to significant AKI and ATN and even several cases of glomerular diseases. Such vaccine associated immune responses should not deter one from getting vaccinated. Overall, even the flu vaccine and other vaccines have been associated with several glomerular diseases such as MCD and membranous nephropathy. Given mass vaccinations happening around the world, there will be cases of vaccine induced GNs( but still very very rare)
Sunday, October 18, 2020
Concept Map: Glomerular Diseases with Immunotherapy
A recent systematic review discussed GNs cases seen with immune checkpoint inhibitors. This concept map( part of the paper) is displayed here.
https://www.kireports.org/article/S2468-0249(20)31640-5/fulltext
Another case of membranous nephropathy(this time PLA2R positive)
Even after addition of the above cases, vasculitis would still be the most common and podocytopathies following that. C3 GN would be the third most common.
Friday, August 21, 2020
Concept Map: Various antigens in Membranous Nephropathy
Saturday, February 29, 2020
Nephrology Learning Bytes
 A pathology report says in the IF section: LINEAR IgG staining
A pathology report says in the IF section: LINEAR IgG stainingUsually the classic disease that is associated with that is
1) Anti GBM disease
But 2 other disorders can also have such staining
2) Fibrillary GN
3) Diabetic Nephropathy
Path image courtesy: Utah webpath



.jpg)