Tuesday, January 28, 2020
Concept map: Copeptin in Natremias
The above figure summarizes the best data on use of serum copeptin level for diagnosis of diabetes inspidus and primary polydipsia. Copeptin derives from the precursor protein of AVP and has been correlated well with AVP production
What about in cases of increased ADH- such as SIADH? Data on that is poor and only one large study of >200+ patients showed that in hypovolemic hyponatremia ( appropriate ADH), the copeptin levels were >84pmol/L ( spec 90%, sens 23%) and SIADH fell in the 10-30pmol/L categories( not helping much) and hypervolemic and diuretic induced fell in 30-65pmol/L category. Use of this test is currently not recommended in diagnosis of increased AVP production disorders.
Finally in patients with nephrogenic syndrome of inappropriate anti diuresis, copeptin levels were are low or suppressed.
This article is an excellent summary of the use of copeptin in Na related disorders
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6850413/
Labels:
concept maps,
copeptin,
natremia
Monday, January 20, 2020
Topic Discussion: Hypertension and TMA- chicken or the egg?
A recent discussion on twitter and ASN Communities has sparked this age old battle if HTN related TMA exists? Some believe that TMA is the initial insult and that leads to endothelial damage and HTN is a symptom and not the disease. Some believe that HTN is the start - leading to sheer stress and endothelial damage and in severe cases-- TMA
Check out the amazing twitter discussion by TMA experts on this topic.
What i found was this amazing image
As one can see in this image- with some data existing on this - that malignant HTN can lead to endothelial dysfunction and some complement activation but not as severe as aHUS.
So if HTN does cause TMA, how does one distinguish that from a complement mediated TMA or aHUS? What if we are missing a mutation or an antibody that we haven't discovered.
1) Kidney biopsy cannot distinguish HTN induced TMA from complement mediated TMA 2) C3 being low is more valuable for an over active complement cascade compared to C5b-9 as even HTN can cause that to be elevated
3)) Doing a fundus exam can help significantly- there is no value in genetic testing in grade 3/4 retinopathy and especially with DBP>130mm Hg 4) No value in genetic testing in those that have a good response to bp control and eventually stabilized kidney function.
5) Ongoing TMA despite bp control and recovering of renal function- likely is then not HTN mediated and additional complement testing should be done.
Does having chronic or acute hypertension cause endothelial damage and TMA or does TMA cause endothelial damage and HTN as a result? @purvasharma821 @KidneyKhanin @VBijol @renalmyeloma @NephRodby @GlassockJ— Kenar Jhaveri (@kdjhaveri) January 15, 2020
Check out the amazing twitter discussion by TMA experts on this topic.
What i found was this amazing image
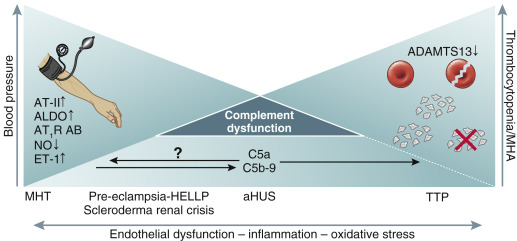
As one can see in this image- with some data existing on this - that malignant HTN can lead to endothelial dysfunction and some complement activation but not as severe as aHUS.
So if HTN does cause TMA, how does one distinguish that from a complement mediated TMA or aHUS? What if we are missing a mutation or an antibody that we haven't discovered.
1) Kidney biopsy cannot distinguish HTN induced TMA from complement mediated TMA 2) C3 being low is more valuable for an over active complement cascade compared to C5b-9 as even HTN can cause that to be elevated
3)) Doing a fundus exam can help significantly- there is no value in genetic testing in grade 3/4 retinopathy and especially with DBP>130mm Hg 4) No value in genetic testing in those that have a good response to bp control and eventually stabilized kidney function.
5) Ongoing TMA despite bp control and recovering of renal function- likely is then not HTN mediated and additional complement testing should be done.
Subscribe to:
Posts (Atom)

