Thursday, July 31, 2014
CONCEPT MAP: Gap acidosis- GOLDMARK
Based on Lancet Article that gives a better ddx for Gap acidosis
http://www.thelancet.com/journals/lancet/article/PIIS0140-6736(08)61398-7/fulltext
Wednesday, July 30, 2014
Topic Discussion: Stones: HEART of the MATTER

Last year, a
prospective study was published in
JAMA suggesting that having a history of kidney stones as an independent
risk factor for cardiac disease (CHD).
In short, this
was a prospective study of 45 748
men and 196 357 women in the United States
without a history of CHD at baseline who were participants in the three study
cohort registries. Coronary heart disease was defined as fatal or nonfatal
myocardial infarction (MI) or coronary revascularization. The outcome was
identified by biennial questionnaires and confirmed through review of medical
records.
Of a total of over
240,000 participants, over 19,000 reported a history of kidney stones. After up
to 24 years of follow-up in men and 18 years in women, 16 838 incident cases of CHD occurred. After adjusting for all
confounders, amongst the 2 cohorts of women, a history of kidney
stones was associated with a modest but statistically significantly increased
risk of CHD; there was no significant association in a separate cohort of men.
The knowledge of history of kidney stones was obtained via an
independently validated survey.
When looking at the covariates, most risk variants of both
formation of kidney stones and CHD were evaluated and controlled for.
Why this risk?
1.
CHD and stone formers share the same risk factors- obesity,
metabolic syndrome, DMII, HTN, high lipids but when controlled for all this,
the risk of getting CHD was independently associated with history of stones
2.
Perhaps common dietary factors- sugary drinks, low calcium diet,
high protein diet, but dietary adjustments were also made in the study.
3.
One adjustment that was not made was renal disease. Stone formers
can perhaps have CKD and CKD becomes then a CHD risk factor. This was not analyzed per authors in the
manuscript.
What is the mechanism?
1.
Perhaps there is a unknown metabolic state that
is both a risk factor for stones and CHD
2.
The stone might increase some other factor that
we don’t know that leads to CHD
3.
There might be some other confounding factor we
haven’t found.
Why Women: -
No clear explanation can be found, perhaps an unknown factor that is not clear
yet.
Major
limitations: Self reported questionnaire, stone analysis not clear, most
patients were white and not many blacks, Asians or Hispanics.
Very
fascinating study but leaves us with more questions than answers. At this point, would not make any major
statements based on this observational study re risk of cardiac disease and
stones.
Monday, July 28, 2014
Cisplatin-induced acute kidney injury (AKI): Why is magnesium balance important?
Cisplatin is one of the most commonly used chemotherapeutic agents. In the US, there are more than 2000 ongoing clinical
trials investigating cisplatin in patients with ovarian, testicular, bladder,
cervical, and head/neck cancers, among others. Unfortunately, approximately 25-30% of
patients receiving cisplatin suffer nephrotoxicity despite its potency as an
anti-tumor agent. This is a challenge in the oncology clinical setting where either
dose reductions or discontinuation of cisplatin are often required to salvage
the kidneys leaving the patient and clinician with limited options given the efficacy
and affordability of this drug. An
important contributor to cisplatin-mediated nephrotoxicity is the accompanying electrolyte
imbalances, including hypomagnesemia. Magnesium (Mg) is an essential dietary mineral
required for normal body functioning and cellular processes. Surprisingly, Mg consumption (via foods and
supplements) among most Americans, particularly the elderly, is below the recommended
daily allowance. In addition, many medications and disease conditions reduce
the availability of dietary Mg. Therefore, we sought to examine the
effects of Mg deficiency and Mg supplementation following Mg deficiency on
cisplatin-mediated acute kidney injury (AKI) using a mouse model. We observed that Mg deficiency exacerbates
cisplatin-induced AKI, whereas correction of Mg status protects against cisplatin-mediated
AKI. Additional studies detail the cellular
and molecular mechanisms by which Mg provides renoprotection, namely by attenuating
cisplatin-induced inflammation, oxidative stress and apoptosis. In addition, we
show for the first time that Mg supplementation reduces the platinum
accumulation in the kidneys possibly by affecting the efflux of cisplatin by
the renal epithelial cells. While
protecting the kidneys, Mg supplementation did not compromise cisplatin-induced
cytotoxicity using several human cancer cell lines, suggesting the Mg does not
interfere with the chemotherapeutic efficacy of cisplatin in vitro. The results of this study warrant future large scale
clinical studies to better monitor patients’ Mg status prior to and during
cisplatin treatment and to develop improved Mg supplementation protocols that
provide nephroprotection without compromising cisplatin’s potent
chemotherapeutic efficacy.
For full link of paper click below
Post By:
Malvika Solanki, MD
Labels:
basic science,
chemotherapy,
magnesium,
onco nephrology
Friday, July 25, 2014
The First Ever Nephrology Spelling Bee
The First Ever Nephrology Spelling Pee Bee
For
the first time ever ( to my knowledge), we conducted a Nephrology Spelling Bee competition
for our residents and trainees. It was
like the ESPN format of the show.
Nephrology faculty prepared tough nephrology entity related words.
Residents were allowed 1 minute to try to spell the word. They could ask 2
questions regarding pronunciation and using it in a sentence. If they got it, they moved to the next round.
If they got it wrong, they got eliminated.
Following the word, a PowerPoint slide was shown with the correct spelling followed by an academic question attached to the word for the trainees. The correct answer to that question would win a nephrology text book. The final spelling bee winner won Tennis US Open tickets.
While
it was a fun event, there was teaching through the academic questions attached
through the words. A surprise host of
the show was Sameer Mishra, prior
national spelling bee winner from 2008( the real deal). Check out his you tube video of the
winning word.
Some
of the words we used were:
amyloidosis,belatacept, podocalyxin, pseudopheochromocytoma to name a
few.
Tuesday, July 22, 2014
Delta –Delta or corrected HCO3- where is this other disorder hiding?
Often when we have a severe gap acidosis, we are forced
to calculate the “delta/delta” and look for either a non gap acidosis or met
alkalosis. How does this work?
Let’s work an example:
Ph 7.1, AG is 22 and serum Hco3 is 10 with a premise of
AG metabolic acidosis.
Method one:
Corrected
bicarbonate = measured bicarbonate +( change in AG)
Corrected
bicarbonate = 10 + (22-12) = 20
If corrected
bicarbonate is <22, a non gap acidosis is present as well
If corrected bicarbonate is >26, a met alk is also present.
If 22-26, a pure gap acidosis remains.
If corrected bicarbonate is >26, a met alk is also present.
If 22-26, a pure gap acidosis remains.
Method two:
Think out loud, “If the AG dropped increased from 12 to 22, there was a change of 10, hence bicarbonate should be roughly down by 10meq. Normal bicarbonate is 24 and hence bicarbonate should be 14, but it’s 10, hence a non gap acidosis is present as well.”
Think out loud, “If the AG dropped increased from 12 to 22, there was a change of 10, hence bicarbonate should be roughly down by 10meq. Normal bicarbonate is 24 and hence bicarbonate should be 14, but it’s 10, hence a non gap acidosis is present as well.”
Most online calculators use this method:
http://www.pharmacologyweekly.com/app/medical-calculators/anion-gap-calculator
http://errolozdalga.com/medicine/pages/AnionGap.DeltaDelta.cr.6.7.10.html
http://errolozdalga.com/medicine/pages/AnionGap.DeltaDelta.cr.6.7.10.html
Problem with this method: Assumptions about all buffering occurring in the ECF and being totally by bicarbonate are not correct. Fifty to sixty percent of the buffering for a metabolic acidosis occurs intracellularly.
Method
three: using the delta-delta ratio
delta
ratio = (Increase in Anion Gap / Decrease in bicarbonate)
delta ratio = ( 10/14)= <1 giving us the same diagnosis of combined gap and non gap acidosis.
See the below table
Delta Ratio
|
Assessment Guideline
|
|
0.4 - 0.8
|
Consider combined high AG & normal AG
acidosis
|
|
1 to 2
|
Usual for uncomplicated high-AG acidosis
Lactic acidosis: average value 1.6 DKA more likely to have a ratio closer to 1 |
|
> 2
|
Suggests a pre-existing elevated HCO3 level so consider: concurrent metabolic
alkalosis
|
As a general rule, in uncomplicated lactic
acidosis, the rise in the AG should always exceed the fall in bicarbonate
level.
The
situation with a pure DKA is a
special case as the urinary loss of ketones decreases the anion gap and this
returns the delta ratio downwards towards one. A further complication is that
these patients are often fluid resuscitated with 'normal saline' solution which
results in a increase in plasma chloride and a decrease in anion gap and
development of a 'hyperchloraemic normal anion gap acidosis' superimposed on
the ketoacidosis. The result is a further drop in the delta ratio.
Ref:
Labels:
acid base,
Consult Rounds,
topic discussions
Monday, July 14, 2014
Diabetic Kidney Disease: Old and New View
A recent
article by Dr Sally
Marshall in ACKD reviews the natural history of CKD in diabetic patients
and reviews the old and the new view of looking at Diabetic Nephropathy. Highly
recommend this article for everyone to review.
Here is a short summary of the review.
Old
view:
Microalbuminuria
is permanent and progresses to proteinuria in most cases.
The peak incidence of DN is 16 years and few after 35 years>
Classically, the microalbumuria progresses to proteinuria and then GFR declines
Usually, this was an older individual disease.
The peak incidence of DN is 16 years and few after 35 years>
Classically, the microalbumuria progresses to proteinuria and then GFR declines
Usually, this was an older individual disease.
New
view:
Low levels of albuminuria( rather than microalbuminuria) is a reversible phenomenon in majority( likely representing more of a hemodynamic change, inflammatory change or endothelial injury rather than structural damage in the kidney)
Higher levels of albuminuria are more likely to progress to proteinuria.
Peak incidence of diseases now ranging from 16-30 years
Atypical forms of presentations are becoming common where GFR decline can be seen without any prior proteinuric variant. A vigilant watch is needed to notice this “non classical” DN
Finally, young adults are being effected with this entity and CKD become more of a common disease in Type 2 DM at an earlier age.
Peak incidence of diseases now ranging from 16-30 years
Atypical forms of presentations are becoming common where GFR decline can be seen without any prior proteinuric variant. A vigilant watch is needed to notice this “non classical” DN
Finally, young adults are being effected with this entity and CKD become more of a common disease in Type 2 DM at an earlier age.
Labels:
asn2011,
CKD and ESRD,
diabetes,
topic discussions
Saturday, July 12, 2014
Clinical Case 83: Answer and Summary
Which one of these drugs is
the most common culprit in acute allergic interstitial nephritis now?
Amoxicillin 13%
Omeprazole 37%
Ciprofloxacin 24%
Ibuprofen 24%
Omeprazole 37%
Ciprofloxacin 24%
Ibuprofen 24%
Classically,
drug induced AIN has been most commonly linked with antibiotics and NSAIDS.
Recently, PPIs have
emerged as a more common cause of AIN than the other drugs. This might be due
to the massive use of these agents for almost all patients that are admitted to
the hospital for ulcer ppx. A recent
study from Mayo Clinic looked at biopsy proven AIN in a single center
retrospectively and identified the culprits. Drugs were 70% of the causes
followed by autoimmune diseases. The most common class of drugs were
antibiotics followed by PPI and then antibiotics. But overall, the top 3 causes
were omeprazole, amoxicillin and then ciprofloxacin. Patients with PPI induced AIN were older, not
as symptomatic and had longer duration of drug exposure till getting kidney
biopsy.
Labels:
acute kidney injury,
Clinical Case,
drug toxicities
Tuesday, July 8, 2014
TOPIC DISCUSSION: Mechanism of Proteinuria in Diabetic Kidney Disease
What is the mechanism behind this entity that we see so
frequently?
If we look at it from different sites of injury, there is
data to support each one of these theories.
Proximal Tubule injury: leading to decreased protein reabsorption
leading to proteinuria.
Hemodynamic injury: leading to glomerular
hyperfiltration leading to increase glomerular pressure and proteinuria
Mesangial cell injury: leads to hypertrophy,
matrix expansion, and mesangiolysis leading to glomerular hypefiltration and
proteinuria
Endothelial cell injury: leading to altered VEGF
leading to podocyte damage
GBM injury: leading to decreased negative charge
and proteinuria
Podocyte injury: leading to podocytopenia or
foot process effacement and leading to apoptosis, degradation or lack of
proliferation.
Vascular insult:- leads to ischemia that can
lead to tubular injury leading to proteinuria.
Which one is primary and which is secondary mechanism? Can diabetic disease progress without
albuminuria? Yes it can.
Current literature supports that diabetic kidney disease is
mainly due to glomerular filtration barrier changes, changes in endothelial
damage and GBM and direct injury to podocytes, Mesangial involvement is more of
secondary role. Tubular interstitial
damage is also playing a role but it the former factors that if disrupted lead
to ongoing proteinuria. This explains
why when we have accelerated HTN on top of diabetic nephropathy, there is
increase in proteinuria likely due to increasing glomerular endothelial damage.
Labels:
diabetes,
proteinuria,
topic discussions
Monday, July 7, 2014
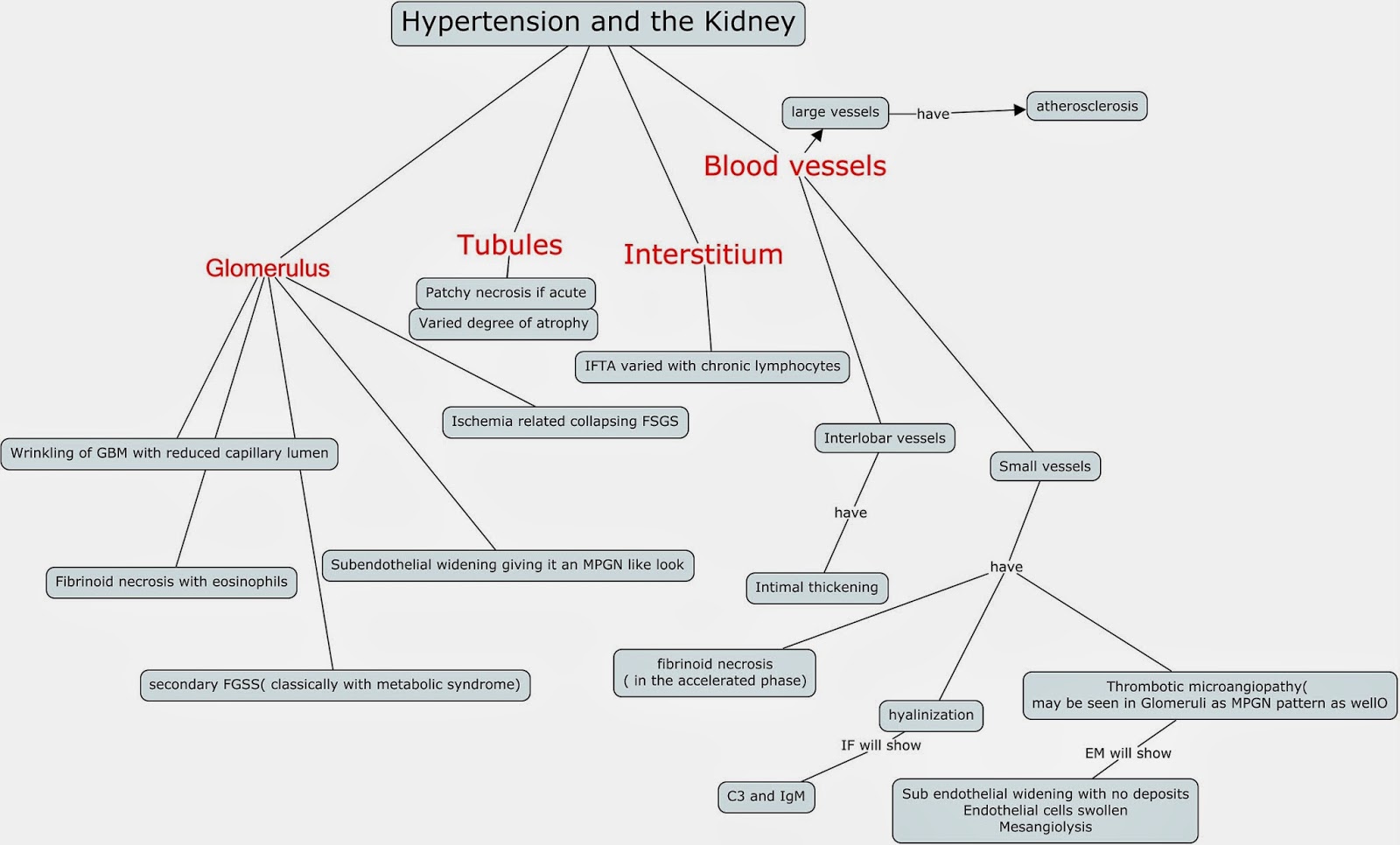
Concept Map: Pathology findings in Hypertension and the Kidney
The different parts of the kidney have classic findings due to HTN. Classically, the glomeruli and vessels are the major targets. The major "disease" categories that are associated with HTN findings are:
FSGS pattern of injury( due to the chronic changes)
Collapsing FSGS form of injury ( due to ischemic injury)
MPGN pattern of injury that is TMA ( negative IF and no deposits)
Here is a good reference
http://www.ncbi.nlm.nih.gov/pubmed/18408477
Labels:
concept maps,
Hypertension,
pathology
Subscribe to:
Comments (Atom)
All Posts
-
▼
2014
(95)
-
▼
July
(9)
- CONCEPT MAP: Gap acidosis- GOLDMARK
- Topic Discussion: Stones: HEART of the MATTER
- Cisplatin-induced acute kidney injury (AKI): Why i...
- The First Ever Nephrology Spelling Bee
- Delta –Delta or corrected HCO3- where is this othe...
- Diabetic Kidney Disease: Old and New View
- Clinical Case 83: Answer and Summary
- TOPIC DISCUSSION: Mechanism of Proteinuria in Diab...
- Concept Map: Pathology findings in Hypertension an...
-
▼
July
(9)