A recent review in ASN Kidney News nicely summarizes the renal function in pregnancy- By Dr.August.
Here are some summary points:
1. GFR will increase by 50%, practical pointers:- crt of 0.4mg/dl is not abnormal and going up to 1.0mg/dl might be a sign of renal dysfunction.
2. Renal Blood Flow increases by 80%
3. There is early decrease in blood pressure to the extent of 5-10mmhg SBP and 2-5mmhg in DBP even letting people come off BP medications
4. There is little evidence that the increased GFR is leading to increased intraglomerular pressures and there is hyperfiltration injury.
5. RR, Tidal Volume and Alveolar ventilation increases in pregnancy
6. Partly compensated resp alkalosis ensues
7. There is a decreased osmotic threshold for thirst and ADH release. Hence, there is a decrease in Serum Osm and plasma Na.
8. Increase 1,25 Vitamin D levels have been observed in Pregnancy and pth is decreased, urinary Ca excretion is decreased.
The last concept is interesting and why these levels increase and perhaps that's the reason we might encounter a slight hypercalcemic state. There is some data that placenta can make pthrp as well.
Interesting physiologic changes
Ref:
ASN KIDNEY NEWS 2011:-Page 7-9
http://www.ncbi.nlm.nih.gov/pubmed/8588110
http://www.ncbi.nlm.nih.gov/pubmed/1992673

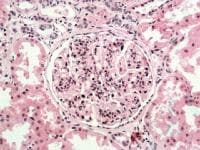

 A commonly used agent is warfarin for anticoagulation. Recently there have been some published case reports of warfarin induced nephropathy(WRN). More recent, an original article on the incidence and prevalence of this entity in CKD has also been mentioned.
A commonly used agent is warfarin for anticoagulation. Recently there have been some published case reports of warfarin induced nephropathy(WRN). More recent, an original article on the incidence and prevalence of this entity in CKD has also been mentioned.