Check out this picture that was created on most cited surgical articles in ten surgical journals.
Turns out Transplantation topics rule and show the most results.
Nice
http://onlinelibrary.wiley.com/doi/10.1111/j.1600-6143.2011.03459.x/full
Pages
▼
Take a look here
▼
Thursday, April 28, 2011
NKF 2011 Live Blogging from Nephrology on Demand
http://nephrologyondemand.org/Blogs from various NKF sessions are now being posted:
TOPIC DISCUSSION: Vascular Amyloidosis and the Kidney
 Most of the pathology in the kidney from AL Amyloidosis is glomerular in origin. Cases have been noted of pure selective amyloid deposition in the vessels walls of different organs. The clinical presentation of renal amyloidosis basically depends on the distribution and severity of amyloid deposits. Vascular localization represents an uncommon pattern of renal amyloidosis, generally associated with chronic renal failure with minimal or no proteinuria.
Most of the pathology in the kidney from AL Amyloidosis is glomerular in origin. Cases have been noted of pure selective amyloid deposition in the vessels walls of different organs. The clinical presentation of renal amyloidosis basically depends on the distribution and severity of amyloid deposits. Vascular localization represents an uncommon pattern of renal amyloidosis, generally associated with chronic renal failure with minimal or no proteinuria. An old series in 1983, of nine patients with secondary (AA type) renal amyloidosis with little or no proteinuria has been reported. Renal failure was the presenting sign of renal disease in seven patients. Renal biopsy revealed a predominantly vascular deposition of amyloid in all patients. Three patients had no glomerular amyloid deposits. This pattern of amyloid deposition was found in 12.5% of our renal biopsies from patient with amyloidosis.
Another recent paper from Japan describes the vascular distribution of amyloid and how that changes when it affects the kidney. This paper looked at patient biopsy samples with AL amyloidosis and divided them into a group with capillary form and a group with small vessel form. The small vessel form was associated with more cardiac involvement, and left ventricular thickening compared to the capillary form. There was no significant differences in rates of survival and renal survival.
In summary, vascular amyloid can been seen in the kidney, usually when you are suspecting it even without nephrotic syndrome.
http://www.ncbi.nlm.nih.gov/pubmed/6839564
http://www.ncbi.nlm.nih.gov/pubmed/20922533
Image Source: http://www.pathconsultddx.com/pathCon/diagnosis?pii=S1559-8675(06)70652-0
Wednesday, April 27, 2011
NKF 2011 Live Blogging: Integrating the treatment of secondary hyperparathyroidism in ESRD
Integrating the treatment of secondary hyperparathyroidism in ESRD
Speaker Dr. Malluche
Blogger: Dr.Azzour Hazzan
Some points from the lecture:1.There are 5 different pth assays assays
2. Have different specificity and sensitivity but the trend is telling and should be trusted.
3.Further using ratio of cap and cip may help (cap is the activating protein within the pth peptide)
4. Using pth you can only screen for high turn over, not diagnose it.
5. Bone volume is also important.
6. Dexa is unreliable and in some cases can give falsely high readings( especially vertebral bones). The hip readings are good
7. Higher bone volume correlates with less calcification in the coronary arteries and vice versa. And that is true with any age.
8. More low turn over with whites along with low volumes
9. More porosis with blacks and high turn over
Speaker Dr. Malluche
Blogger: Dr.Azzour Hazzan
Some points from the lecture:1.There are 5 different pth assays assays
2. Have different specificity and sensitivity but the trend is telling and should be trusted.
3.Further using ratio of cap and cip may help (cap is the activating protein within the pth peptide)
4. Using pth you can only screen for high turn over, not diagnose it.
5. Bone volume is also important.
6. Dexa is unreliable and in some cases can give falsely high readings( especially vertebral bones). The hip readings are good
7. Higher bone volume correlates with less calcification in the coronary arteries and vice versa. And that is true with any age.
8. More low turn over with whites along with low volumes
9. More porosis with blacks and high turn over
TOPIC DISCUSSION: TMA ( AJKD tells the tale of 2 drugs)
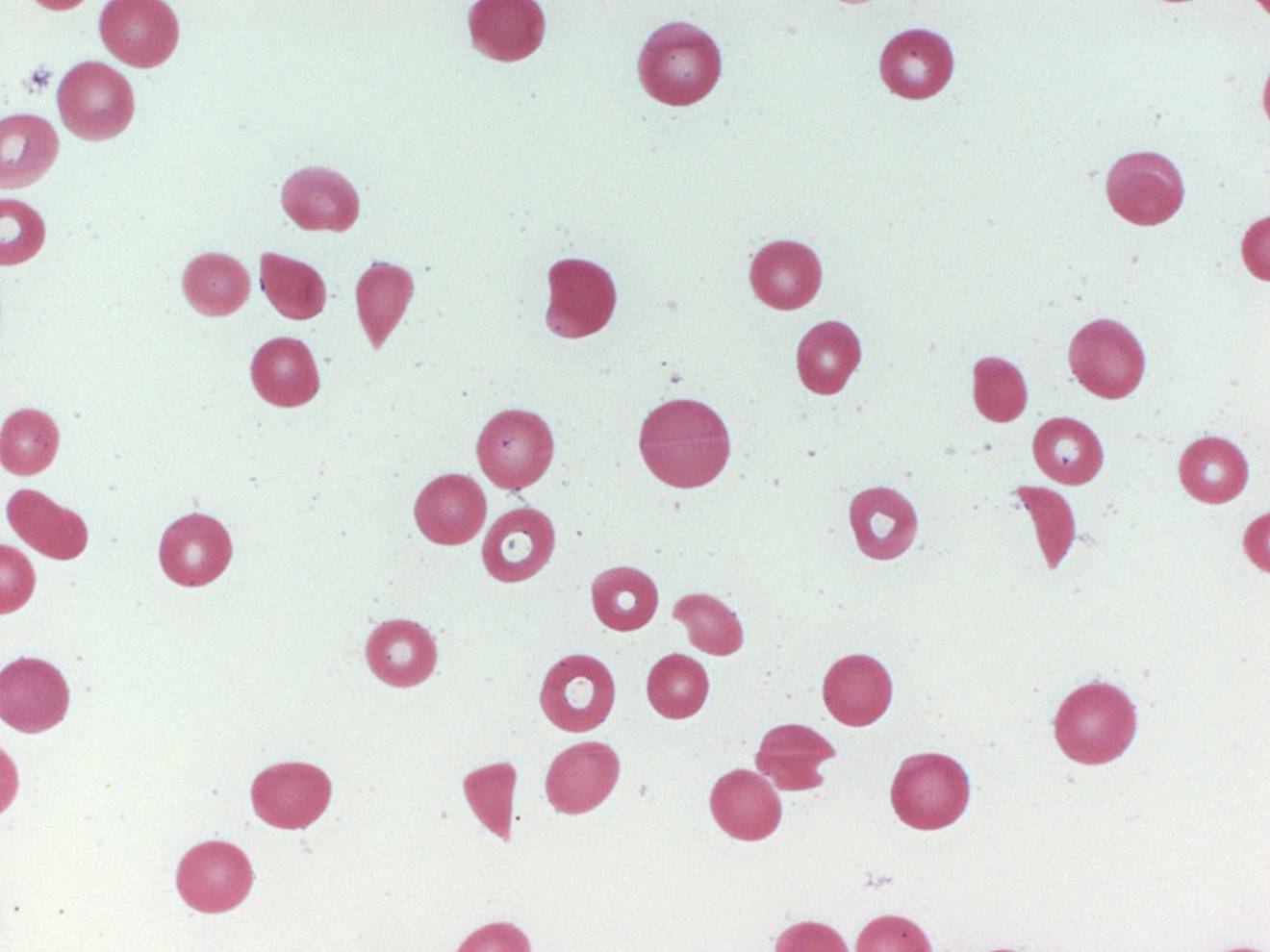 The most recent April 2011 AJKD issue describes two separate manuscripts - both with a diagnosis of TMA.
The most recent April 2011 AJKD issue describes two separate manuscripts - both with a diagnosis of TMA.The first one is acute TMA( biopsy proven) after intraocular administration of anti VEGF agent ( ranibizumab). This is the first case of such an incident. TMA has been associated with systemic treatment with anti VEGF therapy and that has been well documented in the literature. Systemic absorption must be happening regarding this intraocular agents.
The second case is of gemcitabine induced TMA in a vasculitis with granuloma's case presenting with pulmonary renal syndrome but was TMA secondary to the agent and not vasculitis with granulomas. That case illustrates a teaching point of keeping these agents in differential diagnosis of the clinical picture of TMA( low haptoglobin, increased LDH, anemia, hemolysis, schistocytes on smear, worsening HTN, non nephrotic proteinuria, renal dysfunction)
Ref:
http://www.ncbi.nlm.nih.gov/pubmed/21295897
http://www.ncbi.nlm.nih.gov/pubmed/21411201
http://www.ncbi.nlm.nih.gov/pubmed/19203505
http://www.ncbi.nlm.nih.gov/pubmed/21146123
Nephron Animation website
http://www.biologymad.com/resources/kidney.swf
Check out this nice biology resource
Check out this nice biology resource
Tuesday, April 26, 2011
CONSULT ROUNDS: Renal Involvement in Bardet-Biedl syndrome
Bardet-Biedl syndrome (BBS), autosomal recessive, is characterized by rod-cone(retinal) dystrophy (>90%), truncal obesity (72%), postaxial polydactyly, cognitive impairment, male hypogonadotrophic hypogonadism, complex genitourinary malformations, and renal abnormalities and mental retardation. Renal disease is a major cause of morbidity and mortality. This disease entity falls under the category of ciliopathies. The molecular genetic profile of BBS is currently being investigated after the recent identification of 14 BBS genes involved in primary cilia-linked disease. Regular ophthalmologic evaluation, monitoring of renal function and lipid profile, and screening for diabetes mellitus; annual blood pressure measurement
What are the specific renal manifestations of this genetic disease?Renal malformations and abnormal renal function leading to end stage renal disease (ESRD) can be a major cause of morbidity. Renal manifestations include renal dysplasia characterized by malformation of the renal parenchyma and nephronophthisis which often presents with anemia, polyuria, and polydipsia in late childhood. FSGS and glomerular pathology also has been reported. Detrusor instability of the bladder or perhaps even duplication of the collecting system. A recent CJASN article summarized biopsy findings of this disease. This clinical study looked at 33 patients and found that renal abnormalities, including impairment of renal function and signs of chronic interstitial nephropathy of dysplastic nature, were documented in 82% of the patients. Hypertension was found in >30% of the patients and hyperlipidemia in >60%, and almost 50% had other metabolic abnormalities. Interesting, recently in another paper in Kidney International 2011, this disease model was used to study water absorption in the kidney. A cohort of patients with BBS had a urinary concentration defect even when kidney function was near normal and in the absence of major cyst formation. Subsequent in vitro analysis showed that renal cells in which a BBS gene was knocked down were unciliated, but did not exhibit cell cycle defects. The authors state that "As the vasopressin receptor 2 is located in the primary cilium, they studied BBS-derived unciliated renal epithelial cells and found that they were unable to respond to luminal arginine vasopressin treatment and activate their luminal aquaporin 2. The ability to reabsorb water was restored by treating these unciliated renal epithelial cells with forskolin, a receptor-independent adenylate cyclase activator, showing that the intracellular machinery for water absorption was present but not activated. These findings suggest that the luminal receptor located on the primary cilium may be important for efficient transepithelial water absorption."
46% of individuals with this entity have structural renal abnormalities, including calyceal clubbing or calyceal cysts, parenchymal cysts, fetal lobulation and diffuse cortical scarring, unilateral agenesis, and renal dysplasia. Clinical, this can manifest as structural abnormalities include decreased urine-concentrating capacity, renal tubular acidosis, and hypertension, stones and urinary tract infections. Progressive renal impairment frequently occurs in BBS and can lead to end-stage renal disease (ESRD) necessitating renal transplantation in up to 10% of affected individuals.
Image source: uscnk.com
Ref:
- http://www.ncbi.nlm.nih.gov/pubmed/2253248
- http://www.ncbi.nlm.nih.gov/pubmed/3249710
- http://www.ncbi.nlm.nih.gov/pubmed/17604471
- http://www.ncbi.nlm.nih.gov/pubmed/9509476
- http://www.ncbi.nlm.nih.gov/pubmed/20876674
- http://www.ncbi.nlm.nih.gov/pubmed/21270763
- http://www.ncbi.nlm.nih.gov/books/NBK1363/
Monday, April 25, 2011
Dichotomous Effects of Rapamycin
 A recent review in AJT 2011 April issue reviews this concept nicely.
A recent review in AJT 2011 April issue reviews this concept nicely.Rapamycin has many faces and many different effects on different cells. Lets summarize
1. Suppression of CD4 T+ differentiation
2. Increased T reg development
3. Decreased response to skin graft
4. Decreased dendritic cell maturation
5. Increased CD8 + T cell memory differentiation
6. Increased CD8 T cell activation
7. Increased response to pathogen
8. Increased IL-12 production
Commonly noted side effects:- hyperlipidemia, thrombocytopenia, decreased wound healing
Ref and information obtained from:
http://www.ncbi.nlm.nih.gov/pubmed/21446969
TOPIC DISCUSSION: The impact of stopping inhibitors of the renin-angiotensin system in patients with advanced chronic kidney disease.
A recent study in NDT in Dec 2010 discussed this very issue. Inhibition of the renin-angiotensin-aldosterone system (RAAS) has shown to slow chronic kidney disease (CKD) progression. This is most notable at the earlier stages of diabetic and proteinuric nephropathies. What happens and is it beneficial in Stage IV-V and does it prevent faster progression to ESRD. In this study, 12 months after discontinuation of ACEi/ARB eGFR increased significantly to 26.6 ± 2.2 ml/min/ 1.73 m(2) (p = 0.0001). 61.5% of patients had more than a 25% increase in eGFR, whilst 36.5% had an increase exceeding 50%. Overall proteinuria was not affected.
Should we be rethinking this approach? Residual Renal function again comes to mind and how important that might be more than inhibition of RAS.
What do others think?
Ref:
http://www.ncbi.nlm.nih.gov/pubmed/19820248
Should we be rethinking this approach? Residual Renal function again comes to mind and how important that might be more than inhibition of RAS.
What do others think?
Ref:
http://www.ncbi.nlm.nih.gov/pubmed/19820248
Saturday, April 23, 2011
AJP Podcasts
Check out the American Journal of Renal Physiology Podcasts series
http://ajprenal.physiology.org/
Topics:
GFR reduction and acid retention
Albumin as a marker of AKI
ACE-independent intrarenal ANG II formation
http://ajprenal.physiology.org/
Topics:
GFR reduction and acid retention
Albumin as a marker of AKI
ACE-independent intrarenal ANG II formation
Friday, April 22, 2011
IN THE NEWS--> Salt sensitive HTN and temperature?
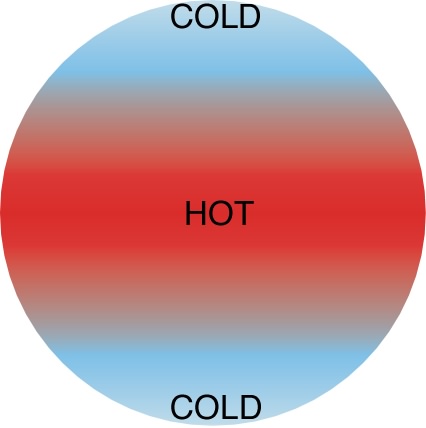 Why are some people having salt sensitive HTN and some don't. A nice study published in HTN Research examines this concept. The researchers examined the effect of salt and water consumption versus just water upon a group of 22 healthy men without high blood pressure. The study participants' blood pressure, rectal temperature, cardiac index and urine output were monitored after the men ingested either salt and water or water alone. Changes in rectal temperature were compared between the men identified as salt sensitive versus those who were salt resistant. The study found that the ingestion of salt and water lowered body temperature more than the ingestion of water by itself. In addition, body temperature decreased more in individuals who are salt resistant than in individuals who are salt sensitive.
Why are some people having salt sensitive HTN and some don't. A nice study published in HTN Research examines this concept. The researchers examined the effect of salt and water consumption versus just water upon a group of 22 healthy men without high blood pressure. The study participants' blood pressure, rectal temperature, cardiac index and urine output were monitored after the men ingested either salt and water or water alone. Changes in rectal temperature were compared between the men identified as salt sensitive versus those who were salt resistant. The study found that the ingestion of salt and water lowered body temperature more than the ingestion of water by itself. In addition, body temperature decreased more in individuals who are salt resistant than in individuals who are salt sensitive. Don't know what to make of these results in a small study. It still begs the question on salt sensitivity is seen in some individuals and some it doesn't apply.
Check out the original study here
http://www.ncbi.nlm.nih.gov/pubmed/21490606
Thursday, April 21, 2011
TOPIC DISCUSSION: Renal Denervation for Treatment Resistant Hypertension: Got the Nerves?
Physiology: Neural Control of Renal Function
An increase in arterial pressure (CO * PR) leads to an increased Una and water excretion via the pressure natriuresis mechanism, with consequent reduction in blood volume until arterial pressure is returned to normal. Factors that decrease renal excretory function and disrupt the above balance by the kidneys lead to an increase in arterial pressure.
Kidney is supplied by T9-T13 nerves leaving the spinal cord and then traversing through sympathetic ganglia to reach the kidney hidden in adventitia of renal vasculature. These nerves are divided into ERSNA (Efferent renal sympathetic Nerve system) to the kidney and afferent nerves from the kidney to the brain (ARSNA). These nerves when fire will cause renal vasoconstriction, increased tubular absorption of sodium, increased Renin Angiotensin System stimulation and reduced GFR (remember these are sympathetic nerves and will do everything they can to maintain/increase blood pressure).
So if you would denervate the kidneys it should result in natriuresis, increased GFR and blood pressure reduction. Cutting the afferent nerve supply to brain would further reduce systemic sympathetic outflow by brain centers.
Trial
Recently, by adrian pharmaceuticals has designed a radiofrequency catheter for ablating nerve supply to renal artery for treatment resistant hypertension.
Multicentre, prospective, randomised trial, patients 18- 85 yrs who had a baseline SBP of 160 mm Hg or more (≥150 mm Hg for patients with type 2 diabetes), despite taking ≥ 3 antihypertensive drugs, were randomly allocated in a one-to-one ratio to undergo renal denervation with previous treatment or to maintain previous treatment alone .
Patients were on average 5.2 medications with e GFR of 77ml/min (many of whom were between 45-60ml/min) were followed for 1 year.
Office based blood pressure measurements in the renal denervation group reduced by 32/12 mm Hg (SD 23/11, baseline of 178/96 mm Hg, p<0.0001), whereas they did not differ from baseline in the control group (change of 1/0 mm Hg [21/10], baseline of 178/97 mm Hg, p=0.77 systolic and p=0.83 diastolic)
Between-group differences in blood pressure at 6 months were 33/11 mm Hg (p<0.0001). At 6 months, 41 (84%) of 49 patients who underwent renal
denervation had a reduction in systolic blood pressure of 10 mm Hg or more, compared with 18 (35%) of 51 controls (p<0.0001).
No serious procedure-related or device-related complications happened.
Occurrence of adverse events did not differ between groups; one patient who had renal denervation had possible progression of an underlying atherosclerotic lesion, but required no treatment.
In Australia and Europe, renal denervation with the Symplicity catheter has received regulator approval and is now entering clinical practice. A US-based trial is planned for the near future, larger than the present one, which will include patients of differing ethnic origin.
Long term follow up at the end of two years should soon be out in press.
CONSULT ROUNDS: Pre Eclampsia
**Preeclampsia usually begins in the third trimester, but can occur earlier in patients with preexisting renal disease or hypertension; as early as 20 weeks.
** It can also occur postpartum with hypertension, even up to 6 weeks after delivery.
**.It presents with weight gain andedema, particularly of the hands and face, proteinuria and HTN. Nephrotic syndrome is noted. Other lab parameters are elevated uric acid, LDH, liver function tests, and can progress to oliguria. Fatty liver of pregnancy, HELLP syndrome, TMA associated with pregnancy all have to be ruled out.
** The severe HTN can itself lead to TMA like picture causing schistocytes to be noted on smear, down-trending haptoglobin and hemolysis ensues.
**There is a fall in renal blood flow and GFR that can lead to hyperuricemia and hypocalciuria as well as acute renal failure. The acute renal failure is thought to be due to glomerular endotheliosis withswelling of endothelial cells and subendothelial hyaline and fibrin deposition. Acute tubular necrosis and cortical necrosis can also occur.
**Pulmonary edema can occur due to changes in pulmonary capillary permeability.
**Hyperreflexia reflects increased nervous system excitability.When preeclampsia is more severe, it can progress to the HELLP syndrome with hemolysis, elevated liver enzymes,and low platelets.
**Due to decreased placental perfusion, fetal growth restriction and oligohydramnios can occur.
For more information take a look at this review for all.
http://www.ncbi.nlm.nih.gov/pubmed/21240869
http://www.ncbi.nlm.nih.gov/pubmed/17261438
** It can also occur postpartum with hypertension, even up to 6 weeks after delivery.
**.It presents with weight gain andedema, particularly of the hands and face, proteinuria and HTN. Nephrotic syndrome is noted. Other lab parameters are elevated uric acid, LDH, liver function tests, and can progress to oliguria. Fatty liver of pregnancy, HELLP syndrome, TMA associated with pregnancy all have to be ruled out.
** The severe HTN can itself lead to TMA like picture causing schistocytes to be noted on smear, down-trending haptoglobin and hemolysis ensues.
**There is a fall in renal blood flow and GFR that can lead to hyperuricemia and hypocalciuria as well as acute renal failure. The acute renal failure is thought to be due to glomerular endotheliosis withswelling of endothelial cells and subendothelial hyaline and fibrin deposition. Acute tubular necrosis and cortical necrosis can also occur.
**Pulmonary edema can occur due to changes in pulmonary capillary permeability.
**Hyperreflexia reflects increased nervous system excitability.When preeclampsia is more severe, it can progress to the HELLP syndrome with hemolysis, elevated liver enzymes,and low platelets.
**Due to decreased placental perfusion, fetal growth restriction and oligohydramnios can occur.
For more information take a look at this review for all.
http://www.ncbi.nlm.nih.gov/pubmed/21240869
http://www.ncbi.nlm.nih.gov/pubmed/17261438
Wednesday, April 20, 2011
Pediatrics Grand rounds continue
Pediatric Nephrology.com continues their grand rounds series that summarizes nephrology news on the web and blogs.
https://pediatric-nephrology.com/index.php?view=entry&year=2011&month=04&day=19&id=462:pgrxvii
https://pediatric-nephrology.com/index.php?view=entry&year=2011&month=04&day=19&id=462:pgrxvii
Tuesday, April 19, 2011
TOPIC DISCUSSION: Hypophosphatemia in Nocturnal hemodialysis
 Hypophosphatemia is observed in patients undergoing nocturnal hemodialysis.
Hypophosphatemia is observed in patients undergoing nocturnal hemodialysis. Why is that? Phos is usually an intra cellular element. When we do regular 3-4 hours of HD, the extraceullar Phos is removed and the intracellular equilibrates and things are in good balance. When things are prolonged in terms of hours ( for the better) in nocturnal HD, there is actually depletion of Phos( seen also in CVVHDF). Many times, this has to be repleted back to the patient to prevent respiratory complications. Phosphate is commonly added to the dialysate acid bath, but systematic evaluation of the safety and reliability of this strategy is lacking. The study linked below looked at the addition of fleet enema to the solution. They added serial aliquots of enema to 4.5 L of dialysate acid concentrate and proportioned the solution on Gambro and Althin/Baxter dialysis machines for up to 8 hours. Then, the dialysate phosphate, Ca, pH, and bicarbonate concentrations at baseline, and after simulated dialysis at 4 and 8 hours was measured. For every 30 mL of Fleet® (1.38 mmol/mL of phosphate) enema added, the dialysate phosphate concentration increased by 0.2 mmol/L. There were no significant changes in dialysate phosphate, Ca, pH, and bicarbonate concentrations over 8 hours. Bacterial and endotoxin testing met sterility standards. The addition of Fleet enema to dialysate increases phosphate concentration in a concentration prediction as depicted above.
Ref:
http://www.ncbi.nlm.nih.gov/pubmed/21395970
http://www.ncbi.nlm.nih.gov/pubmed/21166878
http://www.ncbi.nlm.nih.gov/pubmed/20041960
Image source: periodicfun.wikispaces.com
Monday, April 18, 2011
IN THE NEWS--> Statins and the Kidney after surgery
 A large study in Canada over 200,000 patients over 14 years. The investigators found that people who took statin medications had about a 16% reduced risk of acute kidney injury and a 21% lower risk of dying after their surgeries, compared to people who were not on these agents. Statins appeared to be protective even if patients had been in them a relatively short time, as little as a month or less before surgery.
A large study in Canada over 200,000 patients over 14 years. The investigators found that people who took statin medications had about a 16% reduced risk of acute kidney injury and a 21% lower risk of dying after their surgeries, compared to people who were not on these agents. Statins appeared to be protective even if patients had been in them a relatively short time, as little as a month or less before surgery.Webmd has a complete review:
http://www.webmd.com/cholesterol-management/news/20110414/statin-drugs-cut-risk-kidney-trouble-surgery
Check out the original source at
http://www.ncbi.nlm.nih.gov/pubmed/21493769
Image source: http://www.pharmainfo.net/
Arteries and Kidney Transplant
http://consumer.healthday.com/Article.asp?AID=651907
Check out the news release from JASN
Check out the news release from JASN
Sunday, April 17, 2011
IN THE NEWS -MDR-1 polymorphisms in steroid resistance
Genetics has entered Nephrology with a bang. More and more genetic linkages have allowed for new discoveries to shed light on many glomerular and non glomerular diseases. A recent study in NDT describes the MDR-1 gene expression and P-glycoprotein function with nephrotic syndrome. This is in >200 children study, but sheds an important point. Steroid resistant vs. steroid sensitive. It showed that patients with nephrotic syndrome carrying homozygous mutants of single nucleotide polymorphism (SNP) G2677T/A are prone to develop steroid resistance.
Check it out at:
Saturday, April 16, 2011
TOPIC DISCUSSIONS: Glomerular Disease following congenital cyanotic Heart disease
Glomerular Disease following congenital cyanotic Heart disease (CCHD) is not uncommon. There is fair amount on this in the literature. What do you see on biopsy?
1. Glomerulomegaly
2. Capillary dilatation
3. Thickened capillary walls
4. Focal and diffuse proliferation of mesangial cells
5. Segmental and global glomerular sclerosis
6. Podocyte hypertrophy
7. Proteinuria usually presenting symptom following age 20 or so.
Cause of the damage that has been proposed: increased viscosity, elevated hemotocrit, chronic hypoxia, increased venous pressures, and glomerular hyperfiltration.
Mechanisms: In one study( listed below) , Glomeruli from both kidneys were studied with light microscopy in 13 necropsied cyanotic patients and in 8 controls. The vascular changes were: hilar arteriolar dilatation, capillary diameter, glomerular diameter, and capillary engorgement with red blood cells. The nonvascular changes were : juxtaglomerular cellularity, mesangeal cellularity, mesangeal matrix, focal interstitial fibrosis. There was a significant increase in each of the above vascular and nonvascular items of interest relative to controls. Electron microscopy identified whole megakaryocytes with their cytoplasm in glomeruli. The vascular abnormality is believed to result from intraglomerular release of nitric oxide. The nonvascular abnormality is believed to result from platelet derived growth factor and transforming growth factor beta.
In summary, one sees a FSGS like picture with significant vascular and non vascular changes. Perhaps chronic hypoxia leads to increased Hypoxia induced factor production that might lead to increased VEGF and ultimately FSGS. Not yet studied in these cases. Collapse hasn’t been described in such cases either. Smoking related FSGS might have similar findings and similar findings of glomerulomegaly are also seen in Obesity related FSGS.
Ref:
Image source: healthofchildren.com
Friday, April 15, 2011
Thursday, April 14, 2011
IN THE NEWS:- RENALASE and CKD

What is renalase? A recently discovered enzyme that might be decreased in CKD. It is thought to metabolize catecholamines.
A recent study showed that knock out mice of renalase had increased plasma catecholamine levels and hypertension. It didn't effect plasma BUN and Crt levels. These mice also ended up having increased ventricular hypertrophy and tolerated ischemia poorly. When given recombinant renalase back:- the rescued the cardiac dysfunction.
These are series of papers coming out on Renalase as an enzyme. It might be an interesting concept to keep in mind as it develops perhaps into a possible agent for treatment of HTN in CKD that might have some catecholamine basis.
Take a look:
http://www.ncbi.nlm.nih.gov/pubmed/21178975
http://www.ncbi.nlm.nih.gov/pubmed/21424526
http://www.ncbi.nlm.nih.gov/pubmed/21099685
http://www.ncbi.nlm.nih.gov/pubmed/19471322
Image source:
www.uscnk.com
Wednesday, April 13, 2011
Transplant Tourism and Malignancy
 Transplant Tourism does still continue and many patients continue to get kidneys from other countries where it could be commercial possible. A recent study showed that when groups were compared( tourism kidneys to home country based kidneys):- the graft and patient survivals were equal but the 10 year cumulative cancer risk was significantly higher in the transplant tourism kidneys; especially in the older age group. What might be contributing to this? - immunosuppresive therapy, difficulty in follow ups and were some of the thoughts mentioned in this article. Check it out
Transplant Tourism does still continue and many patients continue to get kidneys from other countries where it could be commercial possible. A recent study showed that when groups were compared( tourism kidneys to home country based kidneys):- the graft and patient survivals were equal but the 10 year cumulative cancer risk was significantly higher in the transplant tourism kidneys; especially in the older age group. What might be contributing to this? - immunosuppresive therapy, difficulty in follow ups and were some of the thoughts mentioned in this article. Check it outRef:
http://www.ncbi.nlm.nih.gov/pubmed/21270768
IN THE NEWS --->Innovative tools in nephrology survey results
 Last year, we had posted a poll regarding some of the innovative teaching tools developed in Nephrology. The results of the poll were presented at ASN 2010 and now in a full article in Kidney international along with description of the tools.
Last year, we had posted a poll regarding some of the innovative teaching tools developed in Nephrology. The results of the poll were presented at ASN 2010 and now in a full article in Kidney international along with description of the tools.Here is the ref:
http://www.ncbi.nlm.nih.gov/pubmed/21451533
Tuesday, April 12, 2011
TOPIC DISCUSSION: Rheumatoid Arthritis and the Kidney
Kidney disease in Rheumatoid Arthritis(RA) is not uncommon. Clinical usually seen with isolated proteinuria, hematuria or both and chronic renal dysfunction as well. Studies have shown that if kidney disease is involved, morbidity and mortality is worse.
Pathogenesis:
1. Immunologic disease:- Non immune complex mediated, immune complex mediated, or pauce immune crescentic GN.
- Immune complex is usually 29% of the diseases, followed by Crescentic GN
- The most common immune complex disease is Membranous GN, Ig A and mesangial GN( usually IgM mediated as RF is IgM)
- Crescentic GN is usually pauce immune ANCA( p ANCA positive), older patients and can be also seen with Anti TNF agents
2. Drug induced:- NSAIDS, Gold, other DMARDS, Anti TNF alpha agents induced disease
- Very important class that can lead to interstitial damage, tubular damage, vascular damage, TMA and GNs.
3. AA Amyloidosis
- very hard to treat. Predictor of mortality in RA.
Ref:
http://www.ncbi.nlm.nih.gov/pubmed/21245821
http://www.ncbi.nlm.nih.gov/pubmed/20617355
http://www.ncbi.nlm.nih.gov/pubmed/20954306
Pathogenesis:
1. Immunologic disease:- Non immune complex mediated, immune complex mediated, or pauce immune crescentic GN.
- Immune complex is usually 29% of the diseases, followed by Crescentic GN
- The most common immune complex disease is Membranous GN, Ig A and mesangial GN( usually IgM mediated as RF is IgM)
- Crescentic GN is usually pauce immune ANCA( p ANCA positive), older patients and can be also seen with Anti TNF agents
2. Drug induced:- NSAIDS, Gold, other DMARDS, Anti TNF alpha agents induced disease
- Very important class that can lead to interstitial damage, tubular damage, vascular damage, TMA and GNs.
3. AA Amyloidosis
- very hard to treat. Predictor of mortality in RA.
Ref:
http://www.ncbi.nlm.nih.gov/pubmed/21245821
http://www.ncbi.nlm.nih.gov/pubmed/20617355
http://www.ncbi.nlm.nih.gov/pubmed/20954306
Monday, April 11, 2011
Saturday, April 9, 2011
CLINICAL CASE 35, ANSWERS AND SUMMARY
Which one of these drugs is associated with Drug Induced Lupus or vasculitis?
Procainamide | 9 (15%) |
Etanercept | 2 (3%) |
Methyldopa | 7 (11%) |
Prophylthiouracil | 3 (5%) |
Methimazole | 0 (0%) |
Furosemide | 1 (1%) |
All except Furosemide | 24 (40%) |
All of them | 10 (16%) |
None of them | 4 (6%) |
Anti-double stranded DNA antibodies are typically absent in drug-induced lupus due to procainamide, hydralazine, and isoniazid, such antibodies are associated with drug-induced disease with other agents, particularly with interferon-alfa and anti-TNF agents. Drug-induced ANCA are sometimes associated with necrotizing vasculitis. Anti-tumor necrosis factor alpha therapy with infliximab, adalimumab, and etanercept has been associated with the development of positive test results for ANA and anti DSdNA.
The renal disease in drug-induced lupus is most often due to a necrotizing glomerulonephritis with little or no immune complex deposition. Usually this is Anti MPO or p ANCA or atypical ANCA( classically in hydralazine). These patients may also have anti-double-stranded DNA antibodies when renal involvement is seen.
Check out the references:
Thursday, April 7, 2011
Wednesday, April 6, 2011
Monday, April 4, 2011
IN THE NEWS- ANCA in the Elderly
The most common glomerular disease in the >80 age group is ANCA associated vasculitis and usually anti MPO in nature. This is now well established. A Recent paper in Kidney International retrospectively looks at treatment of this entity in this age group. Many of us would not treat given the heavy immunosuppresive burden and anticipating increase risk. The investigators in this study, looked at 78 cases that were biopsy proven ANCA vasculitis and showed that the patients with treatment with the agents had a significant lower incidence of ESRD 1 year biopsy with significant p value. No difference in terms of mortality between the two groups in one year. When followed for 2 years, the immunosuppresive group had a better advantage.
Few observations:
Only 35% had extra renal involvement, so most were pure renal involved vasculitis
70% were anti MPO
Majority of them were caucasian
74% female
15% had cancer(at the time diagnosed)
58% of the treated group got Steroids + PO cytoxan
24% got IV cytoxan + steroids, few got MMF
Majority, 34% had no maintenance, Followed by steroids alone and steroids + cytoxan.
Infection was higher in treatment arm.
No particular regimen is suggested from this article, just that immunosuppresion will help in the long run.
Check it out
http://www.ncbi.nlm.nih.gov/pubmed/21160463
Few observations:
Only 35% had extra renal involvement, so most were pure renal involved vasculitis
70% were anti MPO
Majority of them were caucasian
74% female
15% had cancer(at the time diagnosed)
58% of the treated group got Steroids + PO cytoxan
24% got IV cytoxan + steroids, few got MMF
Majority, 34% had no maintenance, Followed by steroids alone and steroids + cytoxan.
Infection was higher in treatment arm.
No particular regimen is suggested from this article, just that immunosuppresion will help in the long run.
Check it out
http://www.ncbi.nlm.nih.gov/pubmed/21160463
Sunday, April 3, 2011
Medicine for residents: Calcium gluconate in a digitalised heart with hype...
Medicine for residents: Calcium gluconate in a digitalised heart with hype...: "Today's morning report was about a young guy who was admitted with rhabdomyolysis, renal failure and hyperkalemia(K- 12mEq/dl) with sine wav..."
Saturday, April 2, 2011
IN THE NEWS--> Detective Nephron's next venture

Check out the april issue of ASN Kidney News 2011 for the next venture of the detective
http://onlinedigeditions.com/publication/?i=65758
Neutropenia from Tacrolimus

Post transplant neutropenia has many causes. Etiology is usually medications, infections, cancer.
In a retrospective evaluation, 28% neutropenia was noted after first year of transplantation. Most of this was sought to be from MMF-tacrolimus combination.
The drugs we usually consider are: MMF, azathioprine, acyclovir, gancyclovir, bactrim, valcyte.
A recent review on CJASN 2011, presents three patients with pure tacrolimus induced neutropenia and the mechanism behind it. All improved after they were switched to cyclosporine.
Why does it happen?
1. Direct inhibition of myeloid cells
2. effect of the drug on mononuclear accessory cells
3. pharmacokinetic interaction between MMF and tacrolimus
4. autoantibodies against myeloid precursors or mature neutrophils
Ref:
http://www.ncbi.nlm.nih.gov/pubmed/21258040
http://www.ncbi.nlm.nih.gov/pubmed/19538494
Friday, April 1, 2011
IN THE NEWS-- Serum Bilirubin and chronic dialysis patients

Here is more data on how perhaps having Gilbert's syndrome might be protective in any medical conditions.
Gilbert sydnrome is a genetic condition that leads to a polymorphism in the activity of the hepatic bilirubin uridine diphosphate-glucuronosyltransferase (UGT1A1). This leads to a slightly elevated indirect bilirubin and otherwise asymptomatic individuals. Many have thought that there might be advantages to having this polymorphism as bilirubin is a natural anti oxidant. Data from other medical diseases have suggested that it might be protective in cardiac, respiratory diseases. Data on renal diseases have been scant except for few recent studies.
A recent study in CJASN 2011, shows a graded reverse association between serum bilirubin and adverse outcomes among chronic hemodialysis patients. the UGT1A1 *28 polymorphism homozygous had significant higher bilirubin levels and hence had one fourth the risk for all cause mortality.
This is fascinating and more studies of these associations should be done. Close to 30% of world population has Gilbert's syndrome and perhaps it is protective in nature!!
Look at a prior post we had:
http://www.nephronpower.com/2010/10/in-news-bilirubin-might-be-protective.html
Ref:
http://www.ncbi.nlm.nih.gov/pubmed/21411679
http://www.ncbi.nlm.nih.gov/pubmed/17895455
http://www.ncbi.nlm.nih.gov/pubmed/20686447
http://www.fedprac.com/asp/archive/article.asp?ArticleID=2209&DeptID=


