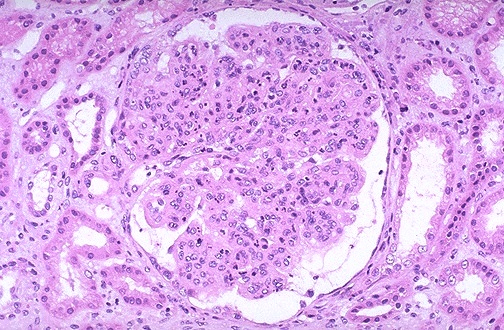
 Pauci immune focal and segmental necrotizing GN guidelines by KDIGO
Pauci immune focal and segmental necrotizing GN guidelines by KDIGO1. Initial treatment( cyclophosphamide and steroids) ( Grade 1A)
2. Rituximab and steroisd be used as alternative when above is contraindicated ( Grade 1B)
3. Plasmapheresis be added if there is rapid rise in crt or on dialysis (Grade 1C)
4. Plasmapheresis be added for pulmonary hemorrhage( Grade 2C)
5. Overlap diseases of ANCA and anti GBM - use plasmapheresis (Grade 2D).
6. If dialysis dependent for 3 months, stop cyclophosphamide if no extra renal manifestations( Grade 2C).
7. Maintenance therapy should be used if achieved remission ( Grade 1B)
8. Continue maintenance therapy for 18 months who achieved remission ( Grade 2D).
9. No maintenance in dialysis dependence and no extra renal manifestations ( Grade 1C)
10. Azathioprine is first choice at 1-2mg/kg/day orally as maintenance therapy ( Grade 1B)
11. MMF up to 1mg BID if above not possible( Grade 2C)
12. Bactrim use as adjunct( Grade 2B)
13. Methotrexate for maintenance if intolerant to azathioprine and MMF if GFR >60 ( Grade 1C)
14. Etanercept should not be used as adjunct therapy ( Grade 1A).
15. Severe Relapse should be treated just like initial disease ( Grade 1C)
16. Other relapses should mean to re starting maintenance therapy ( Grade 2C)
17. Resistant disease:- Rituximab should be used ( 1C), IVIG( 2C) and plasmapheresis (2D)
18. ANCA titer alone should not change therapy ( Grade 2D)
19. Delaying transplantation till complete extrarenal manifestations have been in remission for 12 months( Grade 1C)
20. Not delaying transplantation for those in complete remission but still ANCA positive( Grade 1C).
For full details: http://www.nature.com/kisup/journal/v2/n2/pdf/kisup201226a.pdf
Image source: UNC kidney center website


 KDIGO guidelines are proposed this year in recent Kidney International on glomerular disease.
KDIGO guidelines are proposed this year in recent Kidney International on glomerular disease. KDIGO released guidelines in glomerular diseases in a Kidney International supplement this year.( image source: RFN)
KDIGO released guidelines in glomerular diseases in a Kidney International supplement this year.( image source: RFN)